
With precision medicine, we can now begin to understand who will or who will not respond to immunotherapy. The idea is to essentially take the “guesswork” out of drug selection. Precision medicine allows us to better identify the treatment from which the patient will receive the most benefit. How does precision medicine help identify who could benefit from immunotherapy treatment?

I anticipate that as the technology improves we should also have this down to several days. But with more sophisticated computers even this timeframe is shortening. This is what still takes time and can take up to four weeks to analyze. The complexity comes from the “reading” of the DNA and identifying the abnormal genes. The actual sequencing of the DNA now takes only seconds. We also can make recommendations for clinical trials based on this information, many of which are being conducted at NewYork-Presbyterian. We have a group of specialists who examine gene patterns and then make treatment recommendations based on what is known about the abnormal genes and whether drugs exist to block them. How long does the process take for a patient and what does it entail? With current technology at our cancer centers, we can do the sequencing and the interpretation of the sequencing at a reasonable cost and get this information back to the patient and the patient’s doctor within a few weeks. Twenty years ago, gene sequencing cost millions and took months to receive results. This allows us to understand at a genomic level what is fueling a patient’s cancer to grow. We can do this for every person’s cancer. With the capability to now sequence DNA, we can tell the patient which genes turn cancer on and which genes turn cancer off. How has DNA sequencing allowed doctors to provide personalized cancer care? And how has it evolved over the years? Where we didn’t have treatment options before, we now we have at least two drugs - vemurafenib and dabrafenib - block B-RAF and stop the cancer from growing and spreading.

This gene is mutated in over 60 percent of patients with melanoma. We know now there is one specific gene that is turned on by the sun and sunburn. With this information we have the ability to find a drug that targets that gene, so we can turn the gene off and attack the cancer cell.Ĭan you explain how precision medicine leads us to new therapies for patients?Ī good example of the progress made in outsmarting cancer with precision medicine can be seen in melanoma. By examining the DNA of a patient’s tumor, we can identify the cancer-causing genes that make cancers grow. With precision medicine, we are now in the position to make treatment decisions not simply based on the specific cancer but on the genes that make up that cancer.
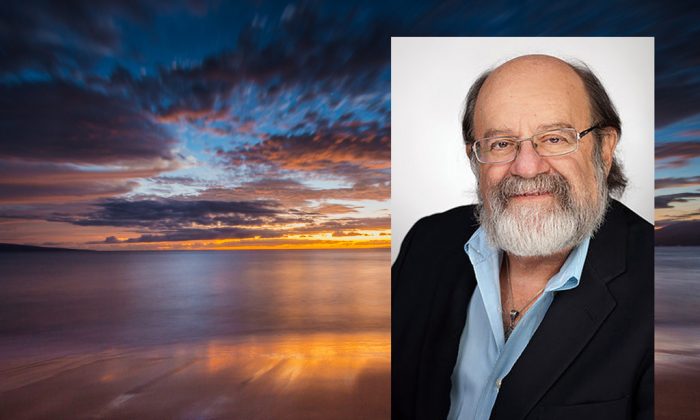
What is the precision medicine approach to treating cancer? Gary Schwartz, chief of the hematology and oncology division at NewYork-Presbyterian/Columbia University Irving Medical Center to understand how treating cancer at the genomic level is having a profound impact on cancer care. At NewYork-Presbyterian and its academic partners, Columbia University Irving Medical Center and Weill Cornell Medicine, clinicians and scientists are using next-generation sequencing tools to gain insight into each patient’s disease. They’re using precision medicine: a strategy in which the patients’ genes provide the clues to potentially defeating their cancer. Today’s oncologists are no longer treating cancer with a one-size-fits-all approach.


 0 kommentar(er)
0 kommentar(er)
